- Case report
- Open access
- Published:
Surgical repair of tetralogy of Fallot in a 78-year-old woman: a case report
Journal of Medical Case Reports volume 18, Article number: 128 (2024)
Abstract
Background
Tetralogy of Fallot is a congenital heart disease mostly diagnosed and treated in early childhood. However, there are some adult cases receiving treatment.
Case presentation
We describe a 78-year-old Japanese woman who presented with severely hypertrophic right ventricle, ventricular septum defect, overriding aorta, and severe infundibular stenosis in the right ventricular outflow tract. As hypoxemia was mild and daily exertion was sufficiently possible, home oxygen therapy was introduced. After 1 month, she was referred because of a positive blood culture. The blood culture test was positive four times, therefore, the antibacterial drug was administered according to active infective endocarditis. SpO2 repeatedly decreased during hospitalization, thus oxygen was needed. As there were infective endocarditis onset and progressive hypoxemia, we planned a surgical correction.
Conclusion
Tetralogy of Fallot was diagnosed and successfully treated with complete surgical correction, and the development of infective endocarditis was the definitive indication for surgery at this late age.
Background
Early surgical correction has been established as the best treatment for tetralogy of Fallot (TOF). Without surgical correction, most patients die during childhood, making adult patients with uncorrected TOF rare. Additionally, surgical indications for untreated adult TOF are mostly due to progression of heart failure [1]. We report an extremely rare case in which intracardiac repair was performed on an elderly cyanotic patient with infective endocarditis.
Presentation of case
The case involved a 78-year-old Japanese woman diagnosed with ventricular septal defect (VSD) during her elementary school days. In her 40s, she felt exertional dyspnea fatigue, but was followed up without any restrictions. At 77 years, she consulted our adult congenital heart disease clinic for increasing symptoms since her 70s. She had a history of hypertension in her 40s and was taking oral calcium channel blockers (nifedipine; 10 mg) and angiotensin receptor blockers (ARBs; candesartan cilexetil; 4 mg) prescribed by a family doctor, and no other previous medical history. Although she had one pregnancy and birth, there were no special events when she gave birth. There was no history of smoking and drinking and no special cardiovascular events in her family history. She has been working as a typist in an office since her 20s.
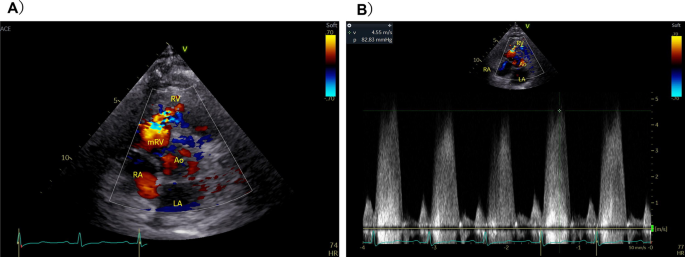
Electrocardiography showed sinus rhythm, right bundle-branch block, and right ventricular hypertrophy with secondary ST–T wave abnormalities. Chest radiography showed an enlarged cardiac silhouette and dilated pulmonary arteries. Transthoracic echocardiography and contrast computed tomography (CT) revealed overriding aorta, right ventricular outflow tract (RVOT) stenosis (Fig. 1), and right ventricular hypertrophy in addition to VSD. The final diagnosis was tetralogy of Fallot (TOF). As hypoxemia was mild and daily exertion was sufficiently possible, home oxygen therapy was introduced after comprehensively explaining the disease and its prognosis.
After 1 month, she was referred from the family doctor and hospitalized because of a positive blood culture test. The physical findings on admission were as follows: body temperature 38.1 ℃, blood pressure 135/71 mmHg, pulse rate 71 beats per minute and regular, and SpO2 87%. Systolic murmur was heard at the left sternal border of the second intercostal space, not rales. No special findings were found on the palpebral conjunctiva, fingers and toes, palms, and soles of the feet. No neurological abnormal findings were observed.
Laboratory findings on admission were as follows: WBC 11,000/μL, Hb 17.5 g/dL, Hct 54%, Plt 19.7/μL, CRP 4.1 mg/dL, AST 24 IU/L, ALT 13 IU/L, LDH 240 IU/L, Na 139 mEq/L, K 3.9 mEq/L, Cl 105 mEq/L, TP 7.0 g/dL, Alb 4.1 mg/dL, BUN 14 mg/dL, Cr 0.59 mg/dL, eGFR 73.1, BNP 88.4 pg/dL, urine specific gravity 1.015, PH 7.0, white blood cell count 0. The blood culture test was positive four times (Lactobacillus rhamnosus) and antibiotic susceptibilities of this bacterium were as follows; penicillin G > 2, aminobenzylpenicillin > 2, ceftriaxone 0.5, gentamicin 1, minocycline 0.25, vancomycin > 16, teicoplanin 16, and levofloxacin 2. Therefore, continuous intravenous administration of ceftriaxone 2 g/day was administered for 6 weeks according to active infective endocarditis. At the time of admission, the patient had a fever of 38 °C, but it remained at 36 °C 3 days after the start of administration. The inflammation data also normalized and negative blood cultures were confirmed twice 3 weeks after starting administration. SpO2 repeatedly decreased to 80% during hospitalization, thus oxygen was started and 3 L was needed to maintain around 90%. Transthoracic echocardiography, thoracic and abdominal CT, head magnetic resonance imaging (MRI), and upper and lower gastrointestinal endoscopy were also performed, but the site or route of infection could not be identified.
Cardiac MRI revealed severe infundibular stenosis and tiny pulmonary valve regurgitation (Additional file 1: Videos S1 and S2), normal right ventricular contractility, 90% normal left ventricular volume, and 0.67 Qp/Qs (pulmonary blood flow/systemic blood flow ratio). As there were progressive hypoxemia and infective endocarditis onset, we planned a surgical correction after infection control of infective endocarditis.
The operation was performed on full cardiopulmonary bypass. The hypertrophic muscle obstructing the RVOT was resected up to 20 mm and the VSD was closed with a patch. A perforation was found in the left semilunar cusp of pulmonary valve and the lesion accompanied by changes in curability was closed directly. The perforation may have been the source of infection. Intraoperative transesophageal echocardiography showed improvement in the RVOT to 2.5 m per second.
Although all follow-up blood culture tests after surgery were negative, ceftriaxone was administered for 4 weeks. The preoperative BNP level of 79 pg/dL increased to 727 pg/dL on day 8 postoperation, but improved to the same preoperative level after oral diuretic discontinuation, and echocardiography revealed normal cardiac function. The patient was discharged on day 35 postoperation at New York Heart Association (NYHA) class I after removing oxygen. It has now been 2 years since the operation, and she is still doing well.
Discussion and conclusion
Early surgical correction has been established as the best treatment for TOF. Without surgical correction, most patients die during childhood [1], making adult patients with uncorrected TOF rare. However, there was a report of uncorrected TOF in the oldest patient aged 86 years [2].
There have been reports of adults with tetralogy of Fallot developing infective endocarditis and brain abscess, but surgical intervention has been avoided [3, 4]. There have only been two reports of repair surgery for tetralogy of Fallot in elderly patients aged 75 years or older, but in both cases the chief complaints were cyanosis and dyspnea [5, 6]. This case of a 78-year-old patient was an extremely rare case in which surgical intervention was indicated due to cyanosis and infective endocarditis.
Most patients with TOF have cyanosis from birth or the first year of life because of right-to-left shunting. If resistance to flow through the RVOT is less than resistance to flow through the aorta, there will be left-to-right shunt flow across the VSD without peripheral cyanosis and there will be a late presentation similarly to our case. Additionally, the patient has suffered from hypertension since her 40s and had high peripheral vascular resistance, which was one possible reason for the delayed cyanosis appearance. Furthermore, hemodynamic evaluation was performed only with four-dimensional (4D) flow MRI, and blood flow evaluation via collateral blood circulation was not considered. Therefore, there may be a discrepancy with the evaluation by cardiac catheterization. Considering the preoperative clinical findings and postoperative left heart failure, we believe that there may have been a large amount of blood flow from small collateral circulation channels.
There have been several reports on the surgical outcome of intracardiac repair for adult TOF. Sadiq et al. showed acceptable morbidity and mortality rates with good long-term surgical outcome [7], whereas Hörer et al. showed a high early mortality rate (15.4%) [8]. Opinions were also divided on the use of transannular patching (TAP), with Sadiq et al. concluding that TAP is not a risk factor, whereas Hörer et al. concluded that TAP is a risk factor [7, 8]. Considering the patient’s life expectancy and the preoperative pulmonary valve annulus system being 20 mm, we decided to form an outflow tract of up to 20 mm without TAP.
Despite the sufficient preoperative left ventricular volume and the restriction of RVOT formation, the increase in the left ventricular volume and pleural effusion after surgery required control of left heart failure. Although premised on improving hemodynamics, it appeared that the strategy for outflow tract formation similar to that in childhood should be reconsidered for the elderly. In our case, we performed complete surgical correction of TOF at 78 years of age, and the development of infective endocarditis was the definitive indication for surgery at rare old age.
Availability of data and materials
Not applicable.
Abbreviations
- VSD:
-
Ventricular septal defect
- RVOT:
-
Right ventricular outflow tract
- TOF:
-
Tetralogy of Fallot
References
Murphy JG, Gersh BJ, Mair DD, Fuster V, McGoon MD, Ilstrup DM, et al. Long-term outcome in patients undergoing surgical repair of tetralogy of Fallot. N Engl J Med. 1993;329:593–9.
Alonso A, Downey BC, Kuvin JT. Uncorrected tetralogy of Fallot in an 86-year-old patient. Am J Geriatr Cardiol. 2007;16:38–41.
Sousa P, Santos W, Marques N, Cordeiro P, Ferrinha R, et al. A 72-year-old woman with an uncorrected tetralogy of Fallot presenting with possible pulmonary endocarditis: a case report. J Med Case Rep. 2013;7:150–3.
Dubey A, Bawiskar N, Kumar S, Lahole S, Somani A. Tetralogy of Fallot—not an innocuous abnormality in adult. J Evolution Med Dent Sci. 2020;16(9):1397–8.
Semeraro O, Scott B, Vermeersch P. Surgical correction of tetralogy of Fallot in a seventy-five year old patient. Int J Cardiol. 2008;128:e98–100.
Hussain FTN, Grogan M, Dearani JA. Surgical repair of tetralogy of Fallot at age 83. World J Pediatr Cong Heart Surg. 2012;3(4):518–20.
Sadiq A, Shyamkrishnan KG, Theodore S, Gopalakrishnan S, Tharakan JM, Karunakaran J. Long-term functional assessment after correction of tetralogy of Fallot in adulthood. Ann Thorac Surg. 2007;83:1790–5.
Hörer J, Friebe J, Schreiber C, Kostolny M, Cleuziou J, Holper K, et al. Correction of tetralogy of Fallot and of pulmonary atresia with ventricular septal defect in adults. Ann Thorac Surg. 2005;80:2285–91.
Acknowledgements
We thank Dr. Edward Barroga (https://orcid.org/0000-0002-8920-2607) for editing the manuscript.
Funding
This study was not funded by any agency or institution.
Author information
Authors and Affiliations
Contributions
YK drafted the original manuscript. SI, TO, and TF substantially contributed to the revisions of the manuscript drafts. All authors have approved the submitted version of the manuscript and agree to be accountable for any part of the work. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Written informed consent was obtained from the patient for the publication of this case report and its accompanying images.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interest associated with this case report.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Video S1:
Magnetic resonance imaging scan of the heart revealing right ventricular outflow tract stenosis (wall shear stress: RA + RV + PA). Video S2: Magnetic resonance imaging scan of the heart revealing right ventricular outflow tract stenosis (energy loss: RA + RV + PA).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Katayama, Y., Isobe, S., Ozawa, T. et al. Surgical repair of tetralogy of Fallot in a 78-year-old woman: a case report. J Med Case Reports 18, 128 (2024). https://0-doi-org.brum.beds.ac.uk/10.1186/s13256-024-04414-5
Received:
Accepted:
Published:
DOI: https://0-doi-org.brum.beds.ac.uk/10.1186/s13256-024-04414-5